'T-UTERUS': let's clarify
Reading Time: 3 minutesThe T-shaped uterus was first described, based on the results of hysterosalpingography, as a congenital uterine anomaly related to diethylstilbestrol (DES), with the shape of the uterine cavity resembling the letter 'T'. Considering the etiology and morphology related to DES, the T-shaped uterus was grouped by the American Fertility Society classification into a separate class of anomalies, without a strict definition or morphometric criteria. However, even following the withdrawal of DES in 1971, the T-shaped uterus continues to be identified although more rarely. The T-shaped uterus may be of primary origin or secondary to intrauterine adhesion syndrome, tuberculosis or adenomyosis.
In 2013, the European Society of Human Reproduction and Embryology/European Society of Gynaecological Endoscopy (ESHRE-ESGE) published guidelines in which the T-shaped uterus was subjectively defined as a narrow uterine cavity due to thickened side walls. It did not specify objective criteria with which to diagnose it nor did it explain how uterine measurements should be performed. The recent official definitions of the American Society for Reproductive Medicine (ASRM) cover only the normal/arched, septate and bicornuate uterus. Until now, no objective and measurable criteria for identifying the T-shaped uterus have been described, and this represents a major obstacle to gathering evidence on its prevalence, clinical implications and optimal management of this morphology. The Congenital Uterine Malformation by Experts (CUME) studied three ultrasound measurements as cut-offs: lateral internal indentation depth ≥ 7 mm, lateral indentation angle ≤ 130° and T angle ≤ 40. In the absence of other abnormalities, they suggest considering a normal uterus when none or only one criterion is met, borderline when two criteria are met and T-shaped when all three criteria are met. These three CUME criteria for defining a T-shaped uterus may help in determining its prevalence, clinical implications and best management and in assessing post-surgical morphological outcome.
However, the diagnosis of the T-shaped uterus remains not straightforward; in the 20th century, the diagnosis of a dysmorphic T-shaped uterus was made by means of hysterosalpingography and two-dimensional ultrasound. As imaging modalities have now improved, with increasing use of 3D ultrasound in gynaecology and reproductive medicine, the detection and diagnosis rates of the T-shaped/dysmorphic uterus have increased. As 3D technology continues to become more accessible and more practitioners become proficient in its use, ultrasound may replace MRI as the new gold standard of reference imaging in the diagnosis of Mullerian anomalies.
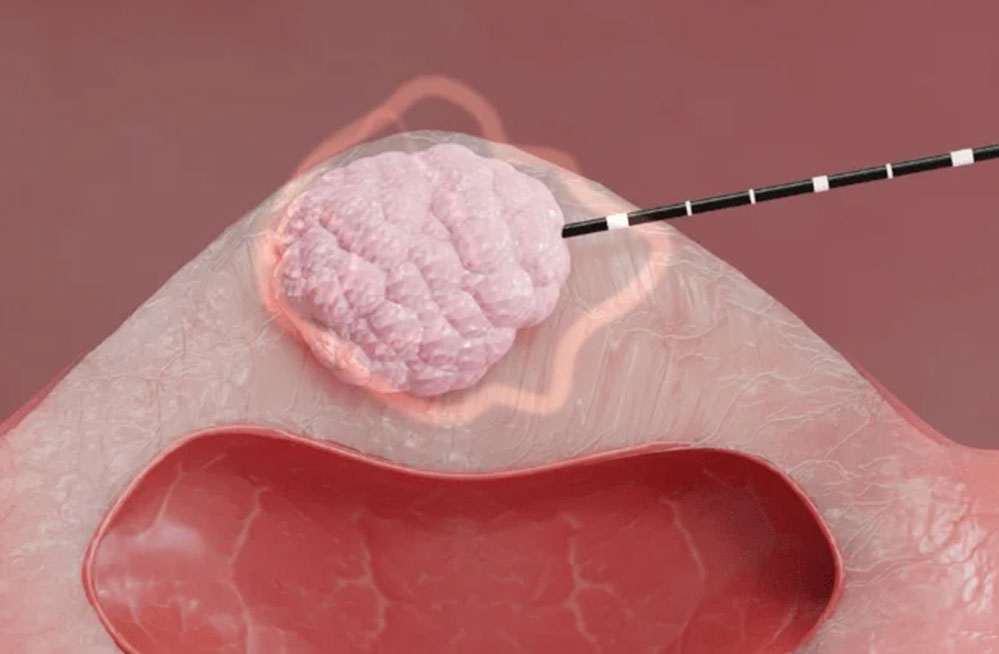
The importance of a correct diagnosis of the T-shaped uterus is linked to the impact that this malformation may have on female fertility. Although, to date, the prevalence does not seem to be that high, a woman's fertility is somehow compromised by this uterine dysmorphism. Correcting abnormal uterine morphology could be the main goal to optimise reproductive results. To date, hysteroscopic correction of the T-shaped uterus may be considered in patients with infertility, polyabortion or repeated failures of in-vitro fertilisation techniques. Hysteroscopic metroplasty is a simple, safe and relatively quick procedure with the advantages of a shorter operating time, a short hospital stay and a reduced incidence of complications compared to the previous laparotomic technique. It is known that subfertility and obstetric complications are more common in women with a dysmorphic uterus than in those with a normal uterine cavity. Despite the absence of large randomised controlled trials, recent data in the literature, however, seem to find better reproductive results after the procedure, configuring hysteroscopic metroplasty as an effective intervention for patients with a T-shaped uterus with fertility intention. Spontaneous pregnancy and term pregnancy rates after surgery have shown promise in these uterine abnormalities.
There is a need for a centralised national/European database for the registration of women with T-shaped uterine anomalies so that meaningful results can be obtained in order to understand the real impact of the T-shaped uterus on women's reproductive lives and its actual prevalence in the population of infertile women. This will also help to define clear diagnostic criteria, indications, surgical techniques and follow-up of reproductive outcomes after the procedure.
References
A Ludwin, et al. Congenital Uterine Malformation by Experts (CUME): diagnostic criteria for T-shaped uterus. Ultrasound Obstet Gynecol. 2020 Jun;55(6):815-829. . Epub 2020 May 15.
Akanksha Sood, et al. T-shaped Uterus in the 21st Century (Post DES era) - We Need to Know More! J Hum Reprod Sci. 2019 Oct-Dec;12(4):283-286. doi: 10.4103/jhrs.JHRS_101_19. Epub 2019 Dec 17.
Antonio La Marca, et al. T-shaped uterus: what has been done, what should be done. Minerva Obstet Gynecol. 2021 Aug;73(4):500-505. doi: 10.23736/S2724-606X.21.04825-9.
Berna Dilbaz, et al. The effect of hysteroscopic metroplasty on fertility in T-shaped and Y-shaped dysmorphic uterus. Eur J Contracept Reprod Health Care. 2022 Oct;27(5):384-389. doi: 10.1080/13625187.2022.2085681. Epub 2022 Jun 21.
Yuxin Zhang, et al. Reproductive outcome of hysteroscopic metroplasty for women with T-shaped uterus: a retrospective study. reprod Health. 2022 Mar 28;19(1):78. doi: 10.1186/s12978-022-01381-2.