OVARIAN ENDOMETRIOMA: WHEN TO OPERATE AND WHEN TO WAIT
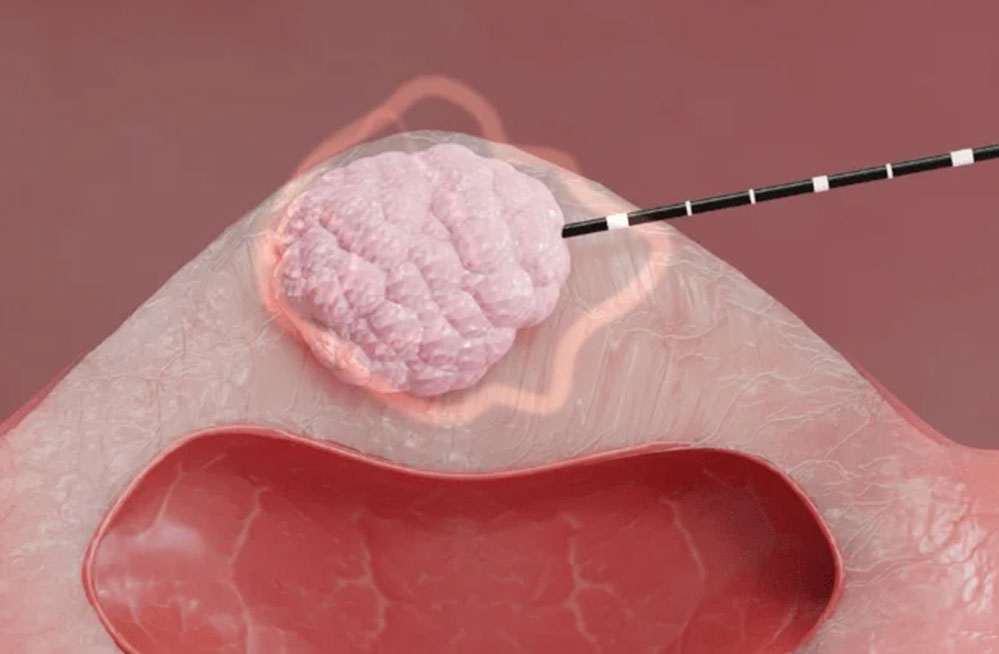
Reading Time: 4 minutesOvarian endometrioma isolated or associated with other lesions is the most common location and manifestation of endometriosis and affects up to 44% of women with the disease. It is a cyst lined by endometrium, itself lined by healthy ovarian parenchyma that is more or less thinned depending on the volume of the cyst. It has a typical cystic content with a 'ground glass' appearance which makes it recognisable and diagnosable on abdominal/transvaginal ultrasound.
Surgery has traditionally been the main treatment option for endometriosis-related infertility of any phenotype. However, advances and refinements in assisted reproductive technologies (ART) allow for a more conservative approach in many scenarios. In patients with reproductive desire, endometrioma resection has been shown to improve natural pregnancy rates. However, the problem arises in patients suffering from infertility who have to resort to the assisted reproduction approach. The very presence of the endometrioma has an impact on fertility and, although surgery can remove the cyst, it may affect the healthy ovarian parenchyma, decreasing the chances of successful assisted reproduction. Anti-Mullerian hormone (AMH), which reflects ovarian reserve, has been shown to decrease after cystectomy, which raises the question of whether endometrioma resection would actually decrease the chances of successful assisted reproduction rather than improve fertility. On the other hand, the persistent presence of an endometrioma could cause problems with egg retrieval and could further contribute to infertility by causing structural changes and disturbances in intraparenchymal circulation.
There is growing molecular, histological and morphological evidence that endometriomas have a detrimental effect on ovarian function. It is not known whether endometrioma reduces the amount of functional tissue available due to space occupation (mechanical stretching damage) or a direct toxic effect. Endometrioma is a peculiar benign cyst without a true capsule. Unlike other benign cysts, endometriotic cyst fluid is capable of inducing oxidative stress in viable cells and potentially causing damage to healthy tissue such as fibrosis, loss of cortical stroma, smooth muscle cell metaplasia, altered vascularisation and, at a later stage, reduced follicular maturation and atresia in early follicles.
In recent meta-analyses it was found that both serum AMH and AFC were reduced in patients with unoperated endometriomas compared to patients with other benign ovarian cysts without endometriosis. Furthermore, in a prospective longitudinal study, a time-dependent effect was recently observed whereby serum AMH decreased faster in women with untreated endometriomas than in healthy controls of the same age. Another major concern is whether surgery has a negative impact on residual ovarian function. Laparoscopic cystectomy of endometriomas has been widely accepted as the gold standard in treatment. The potential detrimental impact of adnexal surgery on ovarian reserve has been studied in several histological studies confirming that cystectomy is generally associated with the inadvertent removal of healthy ovarian tissue and primordial follicles adjacent to the cyst pseudocapsule; this effect increases proportionally to the diameter of the cyst. Unlike other benign cysts, in which a well-defined capsule is present, endometrioma is not surrounded by a capsule and technical difficulties may arise due to the absence of a clear cleavage plane. Despite numerous studies conducted to evaluate the impact of surgical treatment of ovarian endometrioma on ovarian reserve, the data are still inconclusive. There are also discordant outcomes in terms of whether or not AMH and AFC decrease post surgical treatment.
Regarding reproductive outcomes after IVF treatment, recent meta-analyses have shown a lower number of retrieved oocytes in women undergoing surgical treatment for endometrioma than in women with expectant management. Although the data are still controversial, there seems to be an association between surgery and decreased ovarian reserve. In addition, it is hypothesised that surgery may also induce qualitative damage as well as a poorer response to ovarian hyperstimulation during ART. Further clinical analyses implementing standardisation of endometrioma size, bilaterality, surgical technique, postoperative time interval assessments and clinical measurements are needed to help clarify both the contributions and the magnitude of the effect. It appears that in any ovarian surgery there is a compromise of some healthy portion of the ovary, with an inevitable reduction in ovarian follicular reserve, but this certainly varies depending on the type and extent of the pathology, its bilaterality, and the surgeon's skills. Current practice is controversial in the treatment of endometriomas prior to IVF. Guidelines differ from one society to another and the evidence is still not in favour of one management over the other. The guidelines of the European Society of Human Reproduction and Embryology suggest that there is no evidence that cystectomy has a role before IVF techniques in infertile patients with endometriomas. They recommend considering cystectomy in endometriomas > 3 cm to improve pain or accessibility of the follicle. Similarly, surgical treatment is not recommended where the aim is to improve IVF results. They also suggest that drainage may only be considered if the position prevents oocyte retrieval. The American Society of Reproductive Medicine, however, suggests that surgery may improve access to follicles and ovarian response in patients with endometriomas > 4 cm, but states that there is insufficient evidence to imply that success rates will improve. The American College of Obstetricians and Gynecologists and the Society of Obstetricians and Gynecologists of Canada both indicate that surgical management improves infertility outcomes.
In conclusion, when faced with a diagnosis of endometrioma, excision appears to improve spontaneous pregnancy rates in subfertile individuals, but has no impact when advanced reproductive technologies such as in vitro fertilisation are employed. Endometrioma resection has not been shown to improve the results of in vitro fertilisation/intracytoplasmic sperm injection and is therefore not recommended for this indication. The indication remains only in case of symptoms, to exclude malignancy or if the size and/or location of the endometrioma preclude follicle aspiration.
References
Asapoglu I, et al. Endometrioma-related reduction in ovarian reserve: A prospective longitudinal study. Fertil Steril (2018) 110:122-7. doi: 10.1016/j.fertnstert.2018.03.015
Giulia Bonavina and Hugh S. Taylor. Endometriosis-associated infertility: From pathophysiology to tailored treatment. Front Endocrinol (Lausanne). 2022; 13: 1020827. Published online 2022 Oct 26.
Gustavo N Cecchino, et al. Endometrioma, fertility, and assisted reproductive treatments: connecting the dots. urr Opin Obstet Gynecol. 2018 Aug;30(4):223-228. doi: 10.1097/GCO.0000000000000464.
Hamdan M, Dunselman G, Li TC, Cheong Y. The impact of endometrioma on IVF/ICSI outcomes: a systematic review and meta-analysis. Hum Reprod Update 2015; 21:809.
Mauro Busacca, et al. Postsurgical ovarian failure after laparoscopic excision of bilateral endometriomas. m J Obstet Gynecol. 2006 Aug;195(2):421-5. doi: 10.1016/j.ajog.2006.03.064. Epub 2006 May 8.
Mira H Kheil, et al. Endometrioma and assisted reproductive technology: a review. J Assist Reprod Genet. 2022 Feb;39(2):283-290. doi: 10.1007/s10815-022-02403-5. Epub 2022 Jan 24.
Tian Z, et al. Antral follicle count is reduced in the presence of endometriosis: A systematic review and meta-analysis. Reprod BioMed Online (2021) 42:237-47. doi: 10.1016/j.rbmo.2020.09.014