DIAGNOSIS AND TREATMENT OF SPERMATOZOA ABNORMALITIES
Reading Time: 5 minutesInfertility is a major problem in human reproductive health and affects approximately 15% of couples worldwide. Infertility can result from disorders of sexual development or reproductive endocrine disorders with onset in infancy, early childhood or adolescence. Male infertility, which accounts for about half of all infertility cases, is generally manifested by a decrease in the number of spermatozoa called azoospermia or oligozoospermia, decreased sperm motility called asthenozoospermia or an increased percentage of morphologically abnormal spermatozoa, teratozoospermia. These characteristics of spermatozoa, defined in terms of quantity/concentration in the ejaculate, volume, morphology and motility are studied in the analysis of sperm, called spermiogram. Practical sperm analysis follows the recommendations of the WHO laboratory manual for the examination and processing of human sperm. The purpose of sperm analysis is to characterise the male's fertility potential, which is supplemented by clinical and endocrine investigations before a final decision on treatment options is made. In practical terms, performing a detailed macroscopic and microscopic analysis of semen is decisive for obtaining valid results and subsequent treatment decisions. Sperm quality is subject to endocrine and external influences that must be recognised and, if necessary, treated. Regular intake of medication can influence the hormonal control axis (hypothalamic-pituitary-gonadal axis). Acute febrile infections can temporarily impair spermatogenesis and cause reduced sperm quality, which usually returns to normal after 3-6 months. In addition, the period of sexual abstinence affects sperm quality. It is therefore advisable to 'wait' 2 to 5 days before ejaculate diagnosis and to document any deviations from this. Short sexual abstinence of less than 48 hours can lead to a reduction in sperm count; prolonged sexual abstinence of more than 7 days can, for instance, reduce sperm motility. The ejaculate consists of 2 main components: the smaller portion (approx. 5%) comes from the testis and consists mainly of sperm, the larger portion (approx. 95%) is seminal plasma, a mixture of fluid from the epididymis and seminal fluid from the accessory sex glands (prostate and seminal vesicles). The number, motility and morphology of the spermatozoa are the three pillars of the ejaculate evaluation, the standard spermiogram according to WHO also detects the ejaculate volume and pH value, sperm viability, round cells, leucocytes and sperm autoantibodies.
Oligo-astheno-teratozoospermia (OAT) is frequently reported in men from infertile couples. The underlying aetiology of OAT is in most cases unknown and a variety of contributing factors can give rise to the syndrome. According to the definition given by the WHO in the 'WHO Laboratory Manual for the Examination and Treatment of Human Semen' (5th edition, 2010), OAT is defined as a semen sample with: presence of spermatozoa in the ejaculate but the total number below the lower reference limit, percentage of progressively motile (PR) spermatozoa below the lower reference limit and percentage of morphologically normal spermatozoa below the lower reference limit.
As for the proposed treatments, these are based on medical/integrative or surgical pharmacological therapies. These include the proposed treatment with FSH, which may be suggested with little evidence in selected men from infertile couples, normogonadotropic men with idiopathic oligozoospermia or TAO, in an attempt to improve quantitative and qualitative sperm parameters and pregnancy rates. While recombinant (recFSH) or purified human FSH (hpFSH) can be successfully used to treat hypogonadotropic hypogonadism, its application to idiopathic male infertility is more controversial. Anti-estrogens, such as tamoxifen and clomiphene, have been widely used for decades for the treatment of idiopathic male infertility, leading to a significant increase in sperm concentration and motility, in the absence of significant adverse effects. In about half of infertile men, there is an imbalance between oxidative stress and antioxidant capacity in seminal plasma. Reactive oxygen species (ROS) cause damage to sperm membranes through lipid peroxidation, which affects sperm motility and the acrosomal reaction. They also lead to increased DNA fragmentation. In a recent 2011 Cochrane Data Base Systemic Review that included randomised, controlled trials of couples using various antioxidant compounds, a positive impact on live births and pregnancy rates was demonstrated in subfertile couples undergoing ART cycles, but a recent 2014 update of this review concluded "that there is low quality evidence from only small randomised, controlled trials suggesting that antioxidant supplementation in subfertile males may improve live birth rates for couples attending fertility clinics. Low-quality evidence suggests that clinical pregnancy rates may increase. Aromatase inhibitors have been recommended for men with altered sperm parameters and a low testosterone/estrogen ratio. Several small studies using letrozole or anastrozole revealed a significant increase in sperm parameters. Although these results are very promising, this type of treatment cannot currently be recommended in general due to the limited number of studies and the size of the study populations. Finally, androgen treatment regimens cannot be recommended as several meta-analyses failed to show any improvement in pregnancy rates or sperm parameters in men with idiopathic infertility.
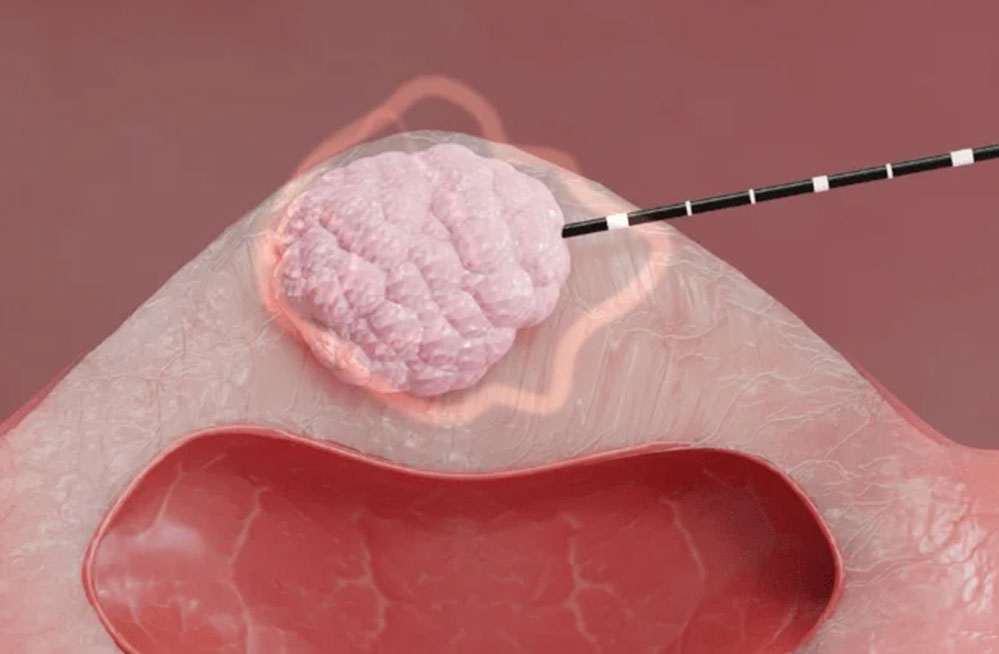
In oligo-astheno-teratozoospermia, surgery may help remove a cause of spermatogenic impairment (such as varicocele), correct distal seminal tract emptying disorders (due to intraprostatic cysts or stenosis of the ejaculatory duct), and improve ICSI results. The treatment of varicocele in infertile couples who report TAO associated with palpable varicocele can be discussed with the couple, considering monitoring only in cases with subclinical varicocele, while treating young males with progressive testicular failure and/or seminal deterioration. The correlation between varicocele (uni- or bilateral) and TAO is controversial, due to its presence both in adult men with normal semen analysis and in men with TAO. Recent meta-analyses show an improvement in sperm quality following palpable varicocele repair, possibly with a higher conception rate after surgery than without surgery and decreased sperm DNA damage. In addition, varicocelectomy may increase total testosterone levels in hypogonadal men with subfertility. In contrast, no significant improvement in postoperative fertility has been demonstrated in TAO cases associated with subclinical varicocele.
So far, there is insufficient evidence from actual interventional studies that lifestyle changes improve male fertility. However, andrologists should advise TAO patients to improve their lifestyle, with additional health benefits; eliminate smoking to increase the couple's chances of achieving the desired pregnancy, reduce weight, reduce alcohol consumption, reduce physical activity if extreme.
It is clear that the possibilities of effectively treating TAO are still rather limited, so in the event that other treatment options are unavailable or ineffective, it is recommended that men with TAO and their partners rely on assisted reproduction techniques to increase their chances of achieving pregnancy.
References
G M Colpi, et al. European Academy of Andrology guideline Management of oligo-astheno-teratozoospermia. Andrology. 2018 Jul;6(4):513-524. doi: 10.1111/andr.12502.
Sabine Kliesch. ["Practical spermiogram"-semen analysis according to WHO recommendations]. Urology A. 2021 May;60(5):647-656. doi: 10.1007/s00120-021-01537-1. Epub 2021 Apr 30.
Shi-Ya Jiao et al. Molecular genetics of infertility: loss-of-function mutations in humans and corresponding knockout/mutated mice. Hum Reprod Update. 2021 Jan 4;27(1):154-189. doi: 10.1093/humupd/dmaa034.